

Ángela Asensio-Martίnez2,3,4 Isabel Blasco-González1,3, Óscar Esteban-Jiménez1, Rosa Magallόn-Botaya1,2,3,4.
1 Aragon Health Service (SALUD). Address: Pº María Agustín, 36. Zip Code: 50071. City: Zaragoza. Country: Spain.
2 University of Zaragoza. Address: Pedro Cerbuna, 12. Zip Code: 50009. City: Zaragoza. Country: Spain.
3 Aragon Institute for Health Research (IIS Aragon). Address: San Juan Bosco, nº13. Zip Code: 50009. City: Zaragoza. Country: Spain.
4. Research Network on Preventive Activities and Health Promotion (RedIAPP). Gran Via de les Corts Catalanes, 587, 08007 Barcelona
Corresponding author: Angela Asensio-Martinez.
Postal address: San Antonio Abad 20, 2ºG. Zip Code: 50010. City: Zaragoza. Country: Spain.
Phone: +34635274038.
Email address: angelacasensio@gmail.com.
Type 2 diabetes, insulinization, primary-care, ethnic
Aims/Introduction: Diabetes mellitus type 2 is a chronic disease which is characterized by a resistance to insulin and the progressive failure of pancreatic beta cells. Today it is one of the most prevalent health problems in developed countries and is considered to be an epidemic.
This paper seeks to evaluate the degree of glycemic control in Diabetes Mellitus Type 2 patients who were treated with oral antidiabetics drugs and who, on account of improper glycemic control, were insulinized as part of standard clinical practice in Primary Attention.
Materials and Methods: Observational, multicenter retrospective study carried out in Primary Healthcare Centers in Aragon, Spain, in 2013. The sample comprised patients of 18 years and over with Diabetes Mellitus Type 2 who were not sufficiently controlled with oral antidiabetic drugs and had needed insulinization.
Results: 151 patients took part in the study. After five months of insulinization there was a statistically significant mean reduction of 1.31 points in HbA1c values, as well as a mean weight loss of 1.24 kg. A logistic regression model was applied for the variables age and sex: females were 2.6 times more likely than men to have an Hba1c>=7% value after being insulinization. The patients expressed a high level of satisfaction with the treatment.
Conclusions: Insulinization is an excellent means of metabolic control for diabetics which can also be used in Primary Healthcare.
Diabetes mellitus type 2 (DM2) is a chronic disease which is characterized by a resistance to insulin and the progressive failure of pancreatic beta cells. This leads to alterations in glucose metabolism which are revealed by an increase in glycemia levels, causing many patients to require insulin therapy to maintain better glycemic control as the disease evolves.
Today it is one of the most prevalent health problems in developed countries and is considered to be an epidemic 1–3. One reason for the increase of the disease is the arrival of migrants from rural areas or abroad, which has led to changes in eating habits and to people abandoning healthier life styles. The disease needs to be fought on all fronts, but first and foremost is prevention. The prevalence of the disease in Spain is put at 13.8% 4. Figures for new cases diagnosed per 1000 people per year range from 8.2 to 10.8 diabetics according to various studies carried out since 2005 5. Prevalence is significantly higher than in European studies, where DM2 in adults stands at 9.1% 6. In Spain, DM2 generates annual direct health costs of €1,305.15 per patient, of which 28.6% is directly related to diabetes control 7.
Some recent studies support the existing evidence for a progressive correlation between glycemia levels and micro and macrovascular diseases, and suggest that the appearance of hyperglycemia may provoke vascular changes in the short term 8,9. A tight control of glycemia is, therefore fundamental in treating diabetes.
According to the figures of glycosylated hemoglobin (HbA1c) from the algorithm for DM2 treatment recently published by the Red de Grupos de Estudio de la Diabetes en Atención Primaria de Salud (redGDPS), the control aims for the disease vary on the basis of age, years of evolution of DM2 and comorbidity 10. The overall aim for patients without complications, with no associated comorbidities and with less than 15 years evolution has an established threshold of 7% of HbA1c. When complications exist and there are more than 15 years of evolution the figure can rise to 8% and in elderly patients with serious comorbidities to 8.5 % 11.
With the new algorithm from the redGDPS for the treatment of hyperglycemia insulin occupies a central point, when previous stages fail, but it can come at any moment of the evolution of the disease when symptoms appear, or if the hyperglycemia intensity so requires 12. Thus, if the control aim is not achieved with metformin, a second oral drug, chosen on an individual basis, is added; if the aim is not achieved with two drugs, a third oral one will be incorporated, basal on insulin or glucagon1like peptide (arGLP1) 12.
If the start or the intensification of the treatment (preferably with insulin) is delayed, this will likely affect the diabetes prognosis unfavorably. A study that evaluated the degree to which patients followed the American Diabetes Association (ADA) Guidelines [10] reported that only 17.2% followed the recommendations therein and just 25% of the patients of the patients at the beginning of the study were not properly controlled (HbA1c>7%). It is clear that the natural progression of DM2 requires close medical monitoring, more intense early insulin therapy and appropriate patient education in order to ensure that the risk of long-term complications, including micro and macrovascular ones, is reduced. However, insulin treatment is commonly postponed, even when bad glycemic control is detected, so it would be advisable to intensify treatment in situations that warrant it.
Recently, Gonzálbez 13 sought to evaluate the degree of metabolic control in patients who had started insulinization on account of bad metabolic control in earlier oral antidiabetic drugs (OADs) treatment and found that the change to insulin improved metabolic control in these patients. The HbA1c mean at the moment of insulinization was 9.2, which fell to 7.87 after 5.7 months of treatment. Moreover, 31.6% of patients had become properly controlled (HbA1c<7).
Notwithstanding the recommendations regarding the benefits of insulinization, there are still many obstacles in the area of Primary Healthcare that mean this type of treatment gets delayed.
This paper seeks to evaluate the degree of glycemic control in patients with Diabetes Mellitus Type 2 who were being treated with OADs and were then insulinized under common Primary Healthcare clinical practice.
An observational, multicenter retrospective study was carried out in Primary Healthcare centers in Aragon, Spain, in 2013 under common clinical practice conditions and in accordance with the ADA and the European Association for the Study of the Diabetes (EASD) consensus. It included patients with DM2 undergoing treatment with OADs and insulin.
Sample and procedure
The reference population comprised patients of 18 years and over with Diabetes Mellitus Type 2 who were not properly controlled with OADs and who needed insulinization.
60 primary healthcare doctors (INDIAN Group) took part in collecting data by sequentially recording all patients at their health centre consultancy who fulfilled the study’s inclusion criteria. These patients were informed about the aims of the study and were asked if they wish to participate. All that did read and signed and informed consent form.
Data were taken from the patients’ clinical records, from interviews with the patient, from the comments made in the patients’ self-analysis diaries and the determinations from the laboratory used by the participating centre.
The main variable was the HbA1c figure, a dichotomy, which was taken as the percentage of patients with an HbA1c < 7% at the time of the visit made in the study. The reason for insulinization was also recorded as were the latest GPA, the existence of episodes of serious hypoglycemia since the beginning of the treatment, cardiovascular risk factors and the degree of patient satisfaction with the anti-diabetes treatment, which was measured using the DTSQ-s (Diabetes Treatment Satisfaction Questionnaire). The questionnaire was designed to measure patients’ satisfaction with their diabetes treatment. It includes eight items to be scored on a scale of zero to six (where 6 = highly satisfied and 0 = not at all satisfied) which measures the following aspects: satisfaction with current treatment (“How satisfied are you with your current treatment?”); convenience of the treatment (“In you recent experience, how practical/comfortable do you consider your treatment to be”); flexibility (“In you recent experience, how flexible would you say your treatment is?”); knowledge of diabetes (“How satisfied are you with your knowledge of your diabetes?”); recommendation of treatment (“Would you recommend your treatment to somebody suffering a similar type of diabetes?”); desire to continue with the treatment (“How satisfied do you feel about continuing your current treatment?”); perceived frequency of hyperglycemia and hypoglycemia (“How often recently have you considered that your sugar level is unacceptably high/low?”) (this item follows a reverse scoring with 6 = most of the time and = = never) 14,15.
The data were statistically analyzed using the statistical program SPSS 20. We began with a descriptive analysis of the data, followed by a comparison of means with Student’s t test. Finally a logistic regression was applied to analyze the main variable, Hba1c, with the rest of the data.
The study was approved by the Aragon Clinical Research Ethics Committee (CEICA) and the Spanish Agency for Medicines and Health Products (AEMPS) as a post-authorization study. All data were collected in accordance with the Spanish Law for the Protection of Data 13/1999, and anonymity and confidentiality were strictly maintained at all times.
151 patients took part in the study of which 63.6% were males and 36.4% females. The mean age was 69.03±10.40 years.
Table 1 shows that prior to insulinization, 4.11% of the subjects presented Hba1c < 7% values and that 95.89% of the sample had a bad control of Hba1c (>=7%). After an average of 5 months following insulinization, 24.66% of the subjects showed a good control of Hba1c (<7%) and 75.34% still had Hba1 values >=7%. Only 31 subjects (21.23%) who showed Hba1c >=7% values prior to insulinization were controlled in the study visit, and 74.66% did not have a good control of Hba1c either before or after insulinization.
In terms of HbA1c values, 90% of the subjects achieved a decrease in Hba1c to a greater or lesser extent when taken as a quantitative variable. An average of 5 months elapsed from the time of insulinization to the control, and a statistically significant (Student’s t test t t= -11.25; p<0.0001) decrease of 1.31 points in HbA1c values had occurred, and there were no differences by sex (Fig. 1).
Mean fasting plasma glucose (GPA) was 140.1 (SD=39.1), with no differences in the GPA value found for sex.
Weight change was measured by comparing pre-insulinization weight with weight at the study visit. Mean weight loss was 1.2 kg (SD=4.7). This decrease was statistically significant (p<0.05) and there were no differences by sex.
As regards cardiovascular risk factors, 23 patients were smokers, 26 were former smokers, 105 were hypertensive (69.5%) and 90 presented dyslipemia (59.6%).
A logistic regression model was made to try to explain the degree of Hba1c control by the demographic variables sex and age, and by the non demographic variables associated to cardiovascular risk: tobacco and HDL, LDL triglycerides consumption, total cholesterol total, Albumin/Creatinine quotient and blood pressure. Data from 87 subjects could be used as these had all these variables previously described. Of these, 70 showed Hba1c >=7% and 17 Hba1c <7%. The model sought the likelihood of occurrence among the variables analyzed at the Hba1c <7% level, but none of the independent variables was able to explain the presence or absence of control of Hba1c. Table 2 gives the relative risk estimates at the 95% confidence level.
A second statistical approach was applied in which a logistic regression model was used only for the demographic variables age and sex. Data from 146 subjects could be used, of which 109 presented Hba1c >=7% and 37 Hba1c <7%. It was observed (Table 3) that the only variable that could explain the control of Hba1c was sex, with an Odds Ratio of 2.63. According to this, women were 2.6 times more likely to have a Hba1c>=7% value than men after insulinization, with a confidence interval of (1.10 – 6.29).
With regard to the hypo and hyperglycemias, 12 subjects reported serious hypoglycemias, 3 cases occurred in one subject, 2 subjects suffered 2 episodes and 8 subjects informed of just one case. Seven of the serious cases of the hypoglycemias were during the night. Of all the patients analyzed, 14.6% showed analytical or symptomatic hypoglycemias after beginning the treatment with insulin.
In order to measure the degree of satisfaction with the prescribed insulinization, the patients were asked to complete questionnaire DTSQ-s 14,15. Scores above 18.5, out of a maximum of 36, denote satisfaction with the treatment. The mean score for the 150 valid cases was 26.8 (SD=4.69), as is shown in Figure 2, thus indicating a high degree of satisfaction. The highest score was 36 and the lowest was 12. Half the subjects scored between 24 and 30 points and 90% scored between 19 and 34. No differences were present by sex.
1. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004 May;27(5):1047–53.
2. WHO | Chapter 6: Neglected Global Epidemics: three growing threats [Internet]. WHO. [cited 2016 Jan 12]. Available from: http://www.who.int/whr/2003/chapter6/en/
3. Hull RL, Westermark GT, Westermark P, Kahn SE. Islet amyloid: a critical entity in the pathogenesis of type 2 diabetes. J Clin Endocrinol Metab. 2004 Aug;89(8):3629–43.
4. Soriguer F, Goday A, Bosch-Comas A, Bordiú E, Calle-Pascual A, Carmena R, et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es Study. Diabetologia. 2012 Jan;55(1):88–93.
5. Ruiz-Ramos M, Escolar-Pujolar A, Mayoral-Sánchez E, Corral-San Laureano F, Fernández-Fernández I. Diabetes mellitus in Spain: death rates, prevalence, impact, costs and inequalities. Gac Sanit SESPAS. 2006 Mar;20 Suppl 1:15–24.
6. IDF diabetes atlas - Home [Internet]. [cited 2016 Feb 24]. Available from: http://www.diabetesatlas.org/
7. Mata M, Antoñanzas F, Tafalla M, Sanz P. The cost of type 2 diabetes in Spain: the CODE-2 study. Gac Sanit SESPAS. 2002 Dec;16(6):511–20.
8. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet Lond Engl. 1998 Sep 12;352(9131):837–53.
9. Grupo de Trabajo Diabetes Mellitus Y Enfermedad Cardiovascular de la Sociedad Española de Diabetes. [Diabetes mellitus and cardiovascular risk. Recommendations of the Working Group of Diabetes Mellitus and Cardiovascular Disease of the Spanish Diabetes Society 2009]. Endocrinol Nutr Órgano Soc Esp Endocrinol Nutr. 2010 May;57(5):220–6.
10. Nuevo Algoritmo de tratamiento de la DM2, de la redGDPS [Internet]. [cited 2016 Jan 12]. Available from: http://www.redgdps.org/index.php?idregistro=948
11. Ismail-Beigi F, Moghissi E, Tiktin M, Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med. 2011 Apr 19;154(8):554–9.
12. Álvarez-Guisasola F, On behalf of the Guiada Study Group. Glycaemic control and implementation of the ADA/EASD-2006 consensus algorithm in type 2 diabetes mellitus patients in primary care in Spain. Int J Clin Pract. 2014 Jan;68(1):28–39.
13. Gonzálbez Morgaez, JD; Ramírez Alcántara, D. Estudio observacional para evaluar el control metabólico en pacientes recientemente insulinizados. Semergen, 2010.
14. Bradley C, Plowright R, Stewart J, Valentine J, Witthaus E. The Diabetes Treatment Satisfaction Questionnaire change version (DTSQc) evaluated in insulin glargine trials shows greater responsiveness to improvements than the original DTSQ. Health Qual Life Outcomes. 2007 Oct 10;5:57.
15. Gomis R, Herrera-Pombo JL, Calderón A, Rubio-Terrés C, Sarasa P. Validación del cuestionario “Diabetes treatment satisfaction questionnaire”(DTSQ) en la población española. PharmacoEconomics Span Res Artic. 2006;3(1):7–18.
16. Maiques Galán A, Brotons Cuixart C, Villar Álvarez F, Navarro Pérez J, Lobos-Bejarano JM, Ortega Sánchez-Pinilla R, et al. Recomendaciones preventivas cardiovasculares. Aten Primaria. 2014;46(Supl.4):3–15.
17. American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care. 2012 Jan;35 Suppl 1:S11-63.
18. Bertoni AG, Krop JS, Anderson GF, Brancati FL. Diabetes-Related Morbidity and Mortality in a National Sample of U.S. Elders. Diabetes Care. 2002 Jan 3;25(3):471–5.
19. Dagogo-Jack S. Preventing diabetes-related morbidity and mortality in the primary care setting. J Natl Med Assoc. 2002 Jul;94(7):549–60.
20. Ministerio de Sanidad, Servicios Sociales e Igualdad - Biblioteca y Publicaciones - Recursos propios - Información terapéutica [Internet]. [cited 2016 Feb 24]. Available from: http://www.msssi.gob.es/biblioPublic/publicaciones/recursos_propios/infMedic/porVolumen/home.htm
21. Mediavilla Bravo JJ. Guías en el manejo de la diabetes mellitus tipo 2. SEMERGEN - Med Fam. 2014 Sep;40:11–8.
22. Santa Cruz NM, Castillo RZ. Tratamiento farmacológico para la diabetes mellitus. Rev Hosp Gen Dr Gea Gonzáles. 2002;5(1):33–41.
23. López-Simarro F, Brotons C, Moral I, Cols-Sagarra C, Selva A, Aguado-Jodar A, et al. Inercia y cumplimiento terapéutico en pacientes con diabetes mellitus tipo 2 en atención primaria. Med Clínica. 2012 Apr;138(9):377–84.
24. DePablos-Velasco P, Salguero-Chaves E, Mata-Poyo J, DeRivas-Otero B, García-Sánchez R, Viguera-Ester P. Calidad de vida y satisfacción con el tratamiento de sujetos con diabetes tipo 2: resultados en España del estudio PANORAMA. Endocrinol Nutr. 2014 Jan;61(1):18–26.
26. Cabrera de León A, Castillo Rodríguez JC del, Domínguez Coello S, Rodríguez Pérez M del C, Brito Díaz B, Borges Álamo C, et al. Estilo de vida y adherencia al tratamiento de la población canaria con diabetes mellitus tipo 2. Rev Esp Salud Pública. 2009.
26. Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, et al. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006 Jan 31;113(4):525–34.
27. Rombopoulos G, Panitti E, Varounis C, Katsinas C, Stefanidis I, Goumenos D. A multi-center, epidemiological study of the treatment patterns, comorbidities and hypoglycemia events of patients with type 2 diabetes and moderate or severe chronic kidney disease - The “LEARN” study. Curr Med Res Opin. 2016 Feb 9;1–43.
28. Pasquel FJ, Powell W, Peng L, Johnson TM, Sadeghi-Yarandi S, Newton C, et al. A randomized controlled trial comparing treatment with oral agents and basal insulin in elderly patients with type 2 diabetes in long-term care facilities. BMJ Open Diabetes Res Care. 2015;3(1):e000104.
29. Confederat L, Constantin S, Lupaşcu F, Pânzariu A, Hăncianu M, Profire L. Hypoglycemia induced by antidiabetic sulfonylureas. Rev Medico-Chir Soc Medici Ş̧i Nat Din Iaş̧i. 2015 Jun;119(2):579–84.
30. Bradley C, Gamsu DS. Guidelines for encouraging psychological well-being: report of a Working Group of the World Health Organization Regional Office for Europe and International Diabetes Federation European Region St Vincent Declaration Action Programme for Diabetes. Diabet Med J Br Diabet Assoc. 1994 Jun;11(5):510–6.
31. Bradley C. Diabetes treatment satisfaction questionnaire. Change version for use alongside status version provides appropriate solution where ceiling effects occur. Diabetes Care. 1999 Mar;22(3):530–2.
|
Table 1. Percentage of patients with poor or good control of Hba1c pre and post insulinization. |
|||
|---|---|---|---|
|
Pre-Insulinization |
Post insulinization |
||
|
|
Hba1c >=7% (53mmol/mol) |
Hba1c <7% (53mmol/mol) |
% Total of Patients |
|
Hba1c <7% (53mmol/mol) |
1 |
5 |
6 |
|
Hba1c >=7% (53mmol/mol) |
109 |
31 |
140 |
|
% Total of Patients |
110 |
36 |
146 |
|
Table 2. Relative risk estimates among independent variables and degree of metabolic control. |
||||||
|---|---|---|---|---|---|---|
|
Effect |
PE |
95% CI |
X2 |
p |
||
|
Age |
1.00 |
0.94 |
1.06 |
0.04 |
0.83 |
|
|
Female/Male |
0.26 |
0.06 |
1.12 |
3.22 |
0.07 |
|
|
Non smoker/Smoker |
1.45 |
0.26 |
7.87 |
0.19 |
0.66 |
|
|
Triglycerides |
1.00 |
0.99 |
1.02 |
1.77 |
0.18 |
|
|
HDL |
1.05 |
0.98 |
1.13 |
2.56 |
0.10 |
|
|
LDL |
1.01 |
0.97 |
1.05 |
0.57 |
0.44 |
|
|
Total cholesterol |
0.97 |
0.92 |
1.01 |
1.66 |
0.19 |
|
|
Systolic BP |
0.94 |
0.88 |
1.00 |
3.00 |
0.08 |
|
|
Diastolic BP |
0.98 |
0.92 |
1.04 |
0.17 |
0.67 |
|
|
AC quotient |
0.98 |
0.94 |
1.02 |
0.36 |
0.54 |
|
|
PE: Point Estimate. CI: confidence interval |
||||||
|
Table 3. Relative risk estimates by sex and age. |
|||||
|---|---|---|---|---|---|
|
Odds Ratio Estimate |
|||||
|
Effect |
PE |
95% CI |
X2 |
p |
|
|
Age |
0.99 |
0.95 |
1.02 |
0.2803 |
0.59 |
|
Sex Female/Male |
2.63 |
1.10 |
6.29 |
4.7599 |
0.02* |
|
*p<0,05. PE: Point Estimate.CI: confidence interval |
|||||
Figure 1. Diferences by sex in the reduction of HbA1c values
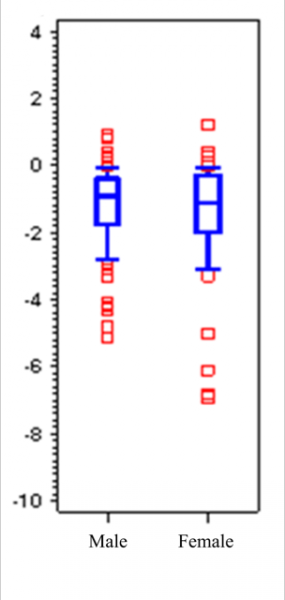
Figure 2. Satisfaction with the treatment (questionnaire DTSQ-s).
..png)